Are you concerned about the new Medicare mandates for Functional Reporting for therapy services in 2013? Are you and your staff fully equipped to manage the change? Do you know which are the best reporting templates?
I've written a new book for physical therapist managers to implement Functional Reporting based on 8 years of experience with self-report measures in my private practice.
This book is for therapists new to functional reporting as well as for therapists who need to gain that extra edge to remain competitive.
I've written this book, pictured in the upper left, for physical therapy managers to implement self-report questionnaires into their clinical workflow. The book was published January 7th, 2012 and it has so far sold well.
I started implementing functional testing systematically in 2005. I had the help of my fellow PTs, physical therapist assistants, administrators, and various support staff. We also started the Physician Quality Reporting Initiative (PQRI) in July 2007, the first year physical therapists were eligible to report.
Chapter One discusses the implementation process, Chapter Two discusses therapist-scored performance measures like the Berg score. The bulk of the book (pp. 73 - 131) describes in detail the self-report tests physical therapists use. I describe 20 self-report tests.
Smart managers will choose the top two or three tests for their high-volume caseloads. Click the link in the upper left to buy the book from the publisher's website at a substantial discount from Amazon. Please e-mail me with any questions you might have.
"Physical therapy is not a subspecialty of the medical profession and physical therapists are not medical doctors; we are a separate profession that provides a unique service that physicians are unable and untrained to provide."
Letter to the AMA from the APTA, Dec 2009
Sunday, December 23, 2012
A Resource for Functional Reporting in 2013 for Physical Therapists
Posted by
Unknown
at
10:48 PM


A Resource for Functional Reporting in 2013 for Physical Therapists
2012-12-23T22:48:00-05:00
Unknown
Functional Reporting|Medicare|physical therapy managers|Physician Quality Reporting Initiative|PQRI|PQRS|
Comments
Labels:
Functional Reporting,
Medicare,
physical therapy managers,
Physician Quality Reporting Initiative,
PQRI,
PQRS
Thursday, December 13, 2012
Live Functional Outcomes Webinar Now at PhysicalTherapy.com
How to Effectively Use Outcomes Questionnaires for Federal Quality Reporting, Better Productivity and Better Outcomes is a recorded webinar that will be also be aired live at PhysicalTherapy.com.
The webinar will start at 8am EST on Thursday, December 13th, 2012.
Membership is required and you can view the recorded webinar at any time, at your convenience.
Get ready for 2013 Functional Reporting or PQRS using standardized outcome measures with How to Effectively Use Outcomes Questionnaires for Federal Quality Reporting, Better Productivity and Better Outcomes.
The webinar will start at 8am EST on Thursday, December 13th, 2012.
Membership is required and you can view the recorded webinar at any time, at your convenience.
Get ready for 2013 Functional Reporting or PQRS using standardized outcome measures with How to Effectively Use Outcomes Questionnaires for Federal Quality Reporting, Better Productivity and Better Outcomes.
Wednesday, December 12, 2012
Answers about Physical Therapy Functional Status Measures
I'm listening to the National Provider Call that covers the new functional reporting requirements for outpatient therapy services, including physical therapy (PT), occupational therapy (OT), and speech language pathology (SLP) services, effective January 1, 2013.
Here is the presentation.
I notice that many of the participants questions that follwoed the presentation are answered in the links provided at the bottom of the National Provider Call-in page. You can go there now and download the material if you haven't already done so.
The new, non-payable G-codes will be a big hurdle for physical therapists, especially the small, outpatient physical therapist who spends his or her whole day treating patients.
I encourage you to review the CMS material. Also, reach out ot your friends and peers to see how they are handling this burden in their practice. E-mail me if I can help at
my e-mail address.
Also, an e-mail mailbox has been created to answer questions related to Functional Status Reporting for Therapy Services at TherapyServicesNPC@cms.hhs.gov.
Here is the presentation.
I notice that many of the participants questions that follwoed the presentation are answered in the links provided at the bottom of the National Provider Call-in page. You can go there now and download the material if you haven't already done so.
The new, non-payable G-codes will be a big hurdle for physical therapists, especially the small, outpatient physical therapist who spends his or her whole day treating patients.
Also, an e-mail mailbox has been created to answer questions related to Functional Status Reporting for Therapy Services at TherapyServicesNPC@cms.hhs.gov.
Posted by
Unknown
at
3:10 PM


Answers about Physical Therapy Functional Status Measures
2012-12-12T15:10:00-05:00
Unknown
cms|Functional Status Reporting|outpatient physical therapist|outpatient therapy services|
Comments
Labels:
cms,
Functional Status Reporting,
outpatient physical therapist,
outpatient therapy services
Sunday, December 9, 2012
Patients Win! Maintenance Therapy Settlement Gets Preliminarily Approval!
Physical therapists' patients can take cheer this holiday season, nestled all snug their beds, with the knowledge that Maintenance Therapy will still be here through Christmas.
The class action lawsuit filed and won by the Center for Medicare Advocacy has tremendous potential to simplify therapy decision making by managers, therapists and patients.
Just in time, too, considering the Byzantine complexity brought by Medicare Manual Reporting and, now, Functional Reporting for 2013.
According to the Center for Medicare Advocacy, on Sunday, December 9th, 2012:
I've had conversations with therapists who support the Improvement Standard on the grounds that "we can't afford to expand Medicare right now".
The Settlement is not an expansion of Medicare. The Settlement is a clarification of the Congressional intent to provide Medicare beneficiaries with a level of care that would not leave them disabled and institutionalized.
For my entire 20-year career, I've been told by well-meaning PT managers and staff that we must "show progress" in order to treat our patients. In turn, my managers had been told by the Medicare Carriers and Fiscal Intermediaries (mainly Blue Cross/Blue Shield and other commercial insurers) that claims would be denied if the patients didn't "show progress".
It turns out that the insurance companies, acting under the aegis of Medicare, were breaking the law.
Here is testimony the the CMA website:
The class action lawsuit filed and won by the Center for Medicare Advocacy has tremendous potential to simplify therapy decision making by managers, therapists and patients.
Just in time, too, considering the Byzantine complexity brought by Medicare Manual Reporting and, now, Functional Reporting for 2013.
According to the Center for Medicare Advocacy, on Sunday, December 9th, 2012:
"A proposed settlement agreement was filed in federal District Court on October 16, 2012. On November 20, Chief Judge Christina Reiss of the District of Vermont signed an order preliminarily approving the settlement agreement.
By December 10, 2012, notice of the settlement will be posted on the websites of numerous organizations, including the seven national organizations that served as plaintiffs in the case, which will alert advocates and beneficiaries to the terms of the settlement."Many observers believe that Medicare will somehow acquit themselves of 35-plus years of illegal behavior and continue to deny care based on the just-overturned "Improvement Standard". The CMA announcement, however, implies that the class participants, not Medicare, are the ones in position to accept or deny the Settlement.
"Class members will be able to file written objections to the settlement.
The court will hold a Fairness Hearing on January 24, 2013 'to determine whether the settlement agreement is fair, reasonable and adequate,' after which it is hoped that the judge will issue an order permanently approving the settlement agreement."The Settlement only applies to the illegal Improvement Standard, or the idea that people must make significant and measurable gains in function in order to continue receiving therapy services. Two further conditions still apply: the services must be of sufficient complexity that a lesser trained provider could not safely perform the care and the patient must still demonstrate that the services are medically necessary.
The Settlement is not an expansion of Medicare. The Settlement is a clarification of the Congressional intent to provide Medicare beneficiaries with a level of care that would not leave them disabled and institutionalized.
For my entire 20-year career, I've been told by well-meaning PT managers and staff that we must "show progress" in order to treat our patients. In turn, my managers had been told by the Medicare Carriers and Fiscal Intermediaries (mainly Blue Cross/Blue Shield and other commercial insurers) that claims would be denied if the patients didn't "show progress".
It turns out that the insurance companies, acting under the aegis of Medicare, were breaking the law.
Here is testimony the the CMA website:
"These changes [from the Settlement] are extremely meaningful, as my mother has repeatedly been denied the ability to continue the physical therapy she needs in order to prevent further deterioration of her condition.
It has been extraordinarily frustrating, and after the last cessation of Physical Therapy and subsequent deterioration actually endangered her life, her quality of life was greatly affected, resulting in extremely expensive 24/7 care.
If she could have kept her PT services, this would not have happened!"
-Veronica, New HampshireIf the Settlement sticks (as I think it will) it will be the best Christmas present of my entire career.
Posted by
Unknown
at
10:59 PM


Patients Win! Maintenance Therapy Settlement Gets Preliminarily Approval!
2012-12-09T22:59:00-05:00
Unknown
Center for Medicare Advocacy|Improvement Standard|maintenance therapy|medically necessary|physical therapy|
Comments
Labels:
Center for Medicare Advocacy,
Improvement Standard,
maintenance therapy,
medically necessary,
physical therapy
Monday, November 5, 2012
Physical Therapist's Private Practice Meeting
WHEN:
Saturday, November 10th, 2012 from 12:00 to 3:00pm
WHERE: Florida Gulfcoast University FGCU School of Physical Therapy in Ft. Myers.
Lunch, drink and snacks sponsored by: A&G Spinal Solutions and Orthopedics, providers of specialized high quality medical Equipment. (Thank you Ryan Williamson).
8695 College Parkway Fort Myers, FL 33919.
Phone: (239) 985-4138)
Meeting will be in Marieb Hall 200, parking is in the adjacent parking garage 4.
WHO: All are welcome to attend - PTs, PTAs, Students, friends, etc.
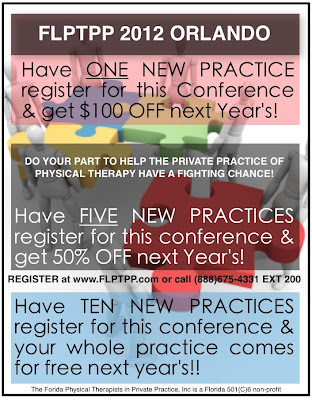
Hosted by Florida Physical Therapists in Private Practice, FLPTPP.com
PURPOSE: This meeting will inform physical therapists and physical therapy students of the immediate issues facing private practioners and physical therapists in all settings regarding healthcare reform. There are many issues currently on the horizon such as the October MedPac report, PIP legislation, and co-pay legislation that is directly impacting our clients access to care and physical therapist reimbursement.
As a group we are banding together with FPTA and our private practice association FLPTPP to effect positive change to allow fair access to clients and compensation. Healthcare reform will happen with the current economic decline and we need to take action or it will happen without us.
Remember if you're not at the table, you're on the menu!
THANK YOU FGCU School of physical therapy and Arie VanDuijn, program director for sponsoring our meeting. We encourage students to attend and have free membership to students in the FLPTPP group to allow them access to current issues.
We also have CEU meetings that students can attend and most recently in Orlando student volunteers attended for FREE!
WHERE: Florida Gulfcoast University FGCU School of Physical Therapy in Ft. Myers.
Lunch, drink and snacks sponsored by: A&G Spinal Solutions and Orthopedics, providers of specialized high quality medical Equipment. (Thank you Ryan Williamson).
8695 College Parkway Fort Myers, FL 33919.
Phone: (239) 985-4138)
Meeting will be in Marieb Hall 200, parking is in the adjacent parking garage 4.
WHO: All are welcome to attend - PTs, PTAs, Students, friends, etc.
Hosted by Florida Physical Therapists in Private Practice, FLPTPP.com
PURPOSE: This meeting will inform physical therapists and physical therapy students of the immediate issues facing private practioners and physical therapists in all settings regarding healthcare reform. There are many issues currently on the horizon such as the October MedPac report, PIP legislation, and co-pay legislation that is directly impacting our clients access to care and physical therapist reimbursement.
As a group we are banding together with FPTA and our private practice association FLPTPP to effect positive change to allow fair access to clients and compensation. Healthcare reform will happen with the current economic decline and we need to take action or it will happen without us.
Remember if you're not at the table, you're on the menu!
THANK YOU FGCU School of physical therapy and Arie VanDuijn, program director for sponsoring our meeting. We encourage students to attend and have free membership to students in the FLPTPP group to allow them access to current issues.
We also have CEU meetings that students can attend and most recently in Orlando student volunteers attended for FREE!
Posted by
Unknown
at
8:13 PM


Physical Therapist's Private Practice Meeting
2012-11-05T20:13:00-05:00
Unknown
FGCU School of physical therapy|Florida Physical Therapists in Private Practice|flptpp|healthcare reform|
Comments
Labels:
FGCU School of physical therapy,
Florida Physical Therapists in Private Practice,
flptpp,
healthcare reform
Thursday, November 1, 2012
A Physical Therapist Won't Forget
Kudos to physical therapist Paul Gaspar, DPT for not giving up...
...for sitting ten hours listening to testimony affecting physical therapy practices in California.
...for rooting out self-serving people, wherever he finds them.
Here's one now...
SomethingaboutMary1st Mailer
...for sitting ten hours listening to testimony affecting physical therapy practices in California.
...for rooting out self-serving people, wherever he finds them.
Here's one now...
SomethingaboutMary1st Mailer
Posted by
Unknown
at
8:28 AM


A Physical Therapist Won't Forget
2012-11-01T08:28:00-04:00
Unknown
california|Paul Gaspar|physical therapist|
Comments
Labels:
california,
Paul Gaspar,
physical therapist
Tuesday, October 23, 2012
Maintenance #PhysicalTherapy Paid by Medicare?
This may be the biggest change to Medicare affecting physical therapists since the March 23rd, 2010 passage of the Patient Protection and Affordable Care Act (PPACA).
Medicare may now be forced to adhere to the statutory language enacted by the Congress instead of the more restrictive policies adopted by individual Medicare Administrative Contractors (MACs) who limited therapy services because the patient did not show progress.
In other words, Medicare may now be forced to pay for "Maintenance Therapy".
A proposed settlement announced today at 2pm by the Center for Medicare Advocacy (CMA) will be held in Washington DC. According to the CMA:
However, the CMA has removed a significant barrier to care between physical therapists and their patients.
What do you think? Are you in favor of Medicare paying for maintenance therapy?
Medicare may now be forced to adhere to the statutory language enacted by the Congress instead of the more restrictive policies adopted by individual Medicare Administrative Contractors (MACs) who limited therapy services because the patient did not show progress.
In other words, Medicare may now be forced to pay for "Maintenance Therapy".
A proposed settlement announced today at 2pm by the Center for Medicare Advocacy (CMA) will be held in Washington DC. According to the CMA:
"Under the agreement, which amounts to a significant change in Medicare coverage rules, Medicare will pay for such services if they are needed to 'maintain the patient’s current condition or prevent or slow further deterioration,' regardless of whether the patient’s condition is expected to improve."Physical therapists have long been told by Medicare Auditors that we must discharge our patients when they "plateau" and their function no longer improves. To be sure, physical therapists shouldn't use today's decision to ignore equally challenging documentation guidelines. Physical therapists still need to show "skilled physical therapy" and "medical necessity for physical therapy". This New York Times article discusses some of the new cost implications to Medicare of maintenance therapy.
However, the CMA has removed a significant barrier to care between physical therapists and their patients.
"For decades, Medicare beneficiaries – particularly those with long-term or debilitating conditions and those who need rehabilitation services – have been denied necessary care based on a so-called “improvement standard.”This decision will impact patients and physical therapists in most settings, including the private practice physical therapy clinic, the home health setting, skilled nursing and the hospital outpatient setting.
This illegal practice means that Medicare coverage for vital care is denied to thousands of individuals on the grounds that their condition is stable, chronic, not improving, or that the necessary services are for “maintenance only”.
The Improvement Standard conflicts with the law."
What do you think? Are you in favor of Medicare paying for maintenance therapy?
Posted by
Unknown
at
2:07 PM


Maintenance #PhysicalTherapy Paid by Medicare?
2012-10-23T14:07:00-04:00
Unknown
Center for Medicare Advocacy|Improvement Standard|maintenance only|maintenance therapy|Medicare coverage|physical therapy|
Comments
Labels:
Center for Medicare Advocacy,
Improvement Standard,
maintenance only,
maintenance therapy,
Medicare coverage,
physical therapy
Monday, October 22, 2012
Medical Apps for Physical Therapy
Video documentation of the physical therapy note is the future and the iPhone is the logical choice for the clinical handset.
Several apps have been developed that use the camera and video features of mobile devices to record patient function.
I reviewed a mobile app developed in 2011 and my review of this innovative mobile app is featured on the Medical App Journal.
Write me if you'd like to see your medical or physical therapy app reviewed.
Several apps have been developed that use the camera and video features of mobile devices to record patient function.
I reviewed a mobile app developed in 2011 and my review of this innovative mobile app is featured on the Medical App Journal.
Write me if you'd like to see your medical or physical therapy app reviewed.
Sunday, October 14, 2012
Important reminders before completing the pre-approval of therapy services form
First Coast Service Options' (First Coast’s) Medical Review department is returning a high volume of pre-approval requests for therapy services forms due to inaccurate, incomplete, or invalid information. Requests that are returned will not be processed. Corrections must be completed and a new request submitted.
The following list has been developed to assist you in avoiding this situation. These are some things you should check for before faxing or mailing your form:
Regardless of whether you receive a confirmation for approval or denial of additional therapy days, once the services are rendered and a claim is submitted, First Coast will request the medical records for review prior to determining whether payment will be made.
The following list has been developed to assist you in avoiding this situation. These are some things you should check for before faxing or mailing your form:
- Verify that you are submitting the pre-approval request during your appropriate phase. Pre-approvals may not be submitted earlier than 15 days prior to the beginning of your applicable phase.
- Do not send in documentation without the completed pre-approval request form.
- Do not use your own coversheet when faxing the pre-approval form. The completed pre-approval form will serve as your coversheet.
- Do not split a single request into multiple faxes. All documentation for a single pre-approval request must be submitted together.
- Do not submit duplicate requests. Physical therapy (PT), occupational therapy (OT), or speech language pathology (SLP) must be checked on the pre-approval form to indicate the therapy discipline that the additional days are being requested for. If a patient is receiving multiple disciplines (e.g., OT, PT) that you are requesting additional therapy days for, two separate requests must be submitted.
- Provide the correct provider transaction access number (PTAN) and/or national provider identifier (NPI) of the applicable facility or individual depending on whether this is for a Part A facility/entity or Part B individual/performing provider. If listing a facility/entity, report the legal business name as reported to the Internal Revenue Service (IRS).
- You must include the name and telephone number of the person to contact regarding the pre-approval request. Providers and therapists that are currently on any type of corrective action (e.g., probe, prepayment review, probe, prepayment review, zone program integrity contractor, etc.) process are not exempt from prepayment review and should consider whether the pre-approval process is beneficial for your office.
Regardless of whether you receive a confirmation for approval or denial of additional therapy days, once the services are rendered and a claim is submitted, First Coast will request the medical records for review prior to determining whether payment will be made.
Posted by
Unknown
at
11:09 AM


Important reminders before completing the pre-approval of therapy services form
2012-10-14T11:09:00-04:00
Unknown
First Coast Service Option|manual medical review|Occupational Therapy|physical therapy|pre-approval of therapy|prepayment review|
Comments
Labels:
First Coast Service Option,
manual medical review,
Occupational Therapy,
physical therapy,
pre-approval of therapy,
prepayment review
Saturday, October 13, 2012
Open Notes Can be Transformational for Physical Therapy
I've been using video to record the patient experience in my outpatient physical therapy clinic for several years. I've never shared that video via the internet with my patient. But, the technology to do that now is simple.
Further, patient functional status, vital signs, objective tests - all these can be shared via the electronic medical record in the physical therapists' clinic.
Watch this video below to see how OpenNotes can change lives and improve health care, including physical therapy:
I posted on OpenNotes here.
Some of the ways I think OpenNotes can help physical therapists include the following:
Do you think OpenNotes of some sort could improve physical therapy?
How?
Please leave a comment.
Further, patient functional status, vital signs, objective tests - all these can be shared via the electronic medical record in the physical therapists' clinic.
Watch this video below to see how OpenNotes can change lives and improve health care, including physical therapy:
I posted on OpenNotes here.
Some of the ways I think OpenNotes can help physical therapists include the following:
- Reduce overblown estimates of "Fraud and Abuse" that are due to good, smart hardworking therapists working in a stupid system.
- Increase patient involvement and compliance with their plan of care.
- Improve therapist productivity that is whittled away working on archaic, frequently handwritten, narrative summaries of the patient experience.
- Pass control and responsibility for the rehabilitative process from the therapist to the patient.
- Increase the role of the "coach" and the "mentor" played by the physical therapist.
- Reduce the administrative burden (currently 100%) borne by the therapist for the creation of the patient record.
Do you think OpenNotes of some sort could improve physical therapy?
How?
Please leave a comment.
Posted by
Unknown
at
11:45 AM


Open Notes Can be Transformational for Physical Therapy
2012-10-13T11:45:00-04:00
Unknown
electronic medical record|OpenNotes|outpatient physical therapy|patient functional status|physical therapist|
Comments
Labels:
electronic medical record,
OpenNotes,
outpatient physical therapy,
patient functional status,
physical therapist
Friday, October 12, 2012
The Incredible Opacity of Physical Therapy
There is no setting more opaque than physical therapy.
Not cardiology. Not orthopedics. Not family practice. Many consumers don't even know what a physical therapist does.
"Did you have study to be a physical therapist?" asked my elderly patient yesterday. I've treated him, on-and-off, for the last four years. The blow-up version of my diploma from the University of Florida (Home of the Fight'n Gators!) occupies about one-third of the wall space in a prominent place in my clinic.
"Yes," I answered gently. "I did study. I went to physical therapy school," I said.
Part of the problem is that even physical therapists don't have a conventional way of describing what we do. Oh, we have jargon. We have "medical-ese". When two physical therapists or therapist assistants talk among themselves the language can get pretty technical - just ask any patient.
"You have a capsular pattern of left shoulder mobility limitation - I don't think it's tendinitis - but instead I think you have adhesive capsulitis."
"Oh," says the patient. "What does that mean?"
The other part of the problem is that physical therapists are trained to write, to record, our findings in a narrative summary that is supposed to describe the patient experience.
The following ridiculous note is the official recommendation of a Medicare auditor in 2009:
Perhaps the answer to the problem of public perception and physical therapists' value can be solved by this out-of-the-box solution: OpenNotes.
OpenNotes has been studied in a new, year-long quasi-experimental study of 13,564 patients just published in the Annals of Internal Medicine:
Not cardiology. Not orthopedics. Not family practice. Many consumers don't even know what a physical therapist does.
"Did you have study to be a physical therapist?" asked my elderly patient yesterday. I've treated him, on-and-off, for the last four years. The blow-up version of my diploma from the University of Florida (Home of the Fight'n Gators!) occupies about one-third of the wall space in a prominent place in my clinic.
"Yes," I answered gently. "I did study. I went to physical therapy school," I said.
Part of the problem is that even physical therapists don't have a conventional way of describing what we do. Oh, we have jargon. We have "medical-ese". When two physical therapists or therapist assistants talk among themselves the language can get pretty technical - just ask any patient.
"You have a capsular pattern of left shoulder mobility limitation - I don't think it's tendinitis - but instead I think you have adhesive capsulitis."
"Oh," says the patient. "What does that mean?"
The other part of the problem is that physical therapists are trained to write, to record, our findings in a narrative summary that is supposed to describe the patient experience.
The following ridiculous note is the official recommendation of a Medicare auditor in 2009:
"Quadriceps strengthening into last 20 degrees of extension with mild manual resistance and proprioceptive cueing, 30 reps to fatigue, continues to decrease current extension lag and improve quality and duration of gait."In the new, patient-centered health care world this narrative from the therapists' perspective is clearly inadequate. Worse, it fails to communicate the value of what physical therapists actually do.
Perhaps the answer to the problem of public perception and physical therapists' value can be solved by this out-of-the-box solution: OpenNotes.
OpenNotes has been studied in a new, year-long quasi-experimental study of 13,564 patients just published in the Annals of Internal Medicine:
"Electronic portals are increasingly used to provide patients with access to their medical records and to interact with the health care system.
In this study of doctors and patients who participated in a 1-year pilot program, most patients reported that the ability to read their doctors’ office notes was beneficial and wanted the program to continue.Some of the benefits of OpenNotes include the following:
Most doctors reported little or no impact on daily workload or patient anxiety or confusion."
- improved doctor-patient relationships
- improved patient satisfaction
- no increase in workload
"At home, patients of the future may review an unedited, automated, 2-camera shoot of a recent electronic or in-person visit to the doctor, and then discuss with family, friends, and the clinician how to modulate and finalize the note.Physical therapists can move forward toward this inspirational vision of the future by beginning to use video notes to record and document their patient experience.
Further ahead, such jointly generated and held records may evolve into a person's story over time, documenting health and illness from early days to the end of life.
We expect that is where we are heading, but on a course filled with fits, starts, and unforeseen consequences. As the patient–doctor relationship moves forward, OpenNotes will almost certainly be on the road ahead."
Thursday, October 4, 2012
Current Hip Replacement Issues
Hip replacement surgery has come under fire recently, chiefly due to issues concerning metal-on-metal replacement systems. Recalls, lawsuits, complications and implant failures have made news in medical circles and even among a number of mainstream news outlets.
If your doctor has recommended replacement surgery to treat your hip trouble or you have already had an implant procedure, you're probably quite interested in finding out exactly what the controversy is all about and how all these problems are happening.
Problems and Complications
Rates of early implant failure were high among these recalled hip replacement systems, forcing many patients to undergo painful and costly surgical procedures, called revisions, to remove the faulty implants, repair the damage and install a new replacement system.
The Recalls
Over the past few years, metal-on-metal hip replacement systems made by several manufacturers have been recalled due to higher than normal rates of complications and premature implant failures.
DePuy Orthopaedics, which is a division of Johnson & Johnson, recalled its ASR Hip Resurfacing System and ASR XL Acetabular System. Two implant products made by Stryker Orthopaedics were recalled: the Rejuvenate and the ABG II modular-neck hip stems. Zimmer Holdings recalled its Durom Cup temporarily, returning it to the market with revised instructions, and Smith & Nephew recalled a component of its R3 Acetabular System.
Implant debris is the source of some of the more serious complications seen with these products, shed due to the friction between components as the patient walks. In the recalled replacement systems, design flaws and improper alignment of the components caused more wear and debris than is usual in hip implants, leading to high rates of debris-related complications and revision surgeries.
Among the most serious of these hip replacement complications is metallosis, which occurs when the soft tissues around the implant are contaminated with metallic debris particles. This can lead to severe pain and inflammation, tissue death, and bone death, often causing implant loosening and failure. In some cases, high levels of metal ions were also found to be circulating in the blood system, disbursed throughout the body. The long-term consequences of that widespread metal contamination in the body have yet to be determined. However, the U.S. Food and Drug Administration (FDA) states that metal ions in the blood can cause other symptoms or illnesses in the nervous system, thyroid gland and heart.
FDA Information and Recommendations
The FDA cautions that patients who have metal-on-metal hip replacements should watch for symptoms that include pain in the groin or leg, swelling at or near the hip joint and a limp or change in walking ability. If these symptoms emerge, patients should be thoroughly examined, and may need testing, including imaging tests, joint aspiration and blood tests to measure levels of metal ions in the blood. The agency also recommends that patients watch for general health symptoms, such as chest pain, shortness of breath, changes in vision or hearing, numbness or weakness, weight gain, fatigue and changes in urinary function.
Elizabeth Carrollton writes about defective medical devices and dangerous drugs for Drugwatch.com.
If your doctor has recommended replacement surgery to treat your hip trouble or you have already had an implant procedure, you're probably quite interested in finding out exactly what the controversy is all about and how all these problems are happening.
Problems and Complications
Rates of early implant failure were high among these recalled hip replacement systems, forcing many patients to undergo painful and costly surgical procedures, called revisions, to remove the faulty implants, repair the damage and install a new replacement system.
The Recalls
Over the past few years, metal-on-metal hip replacement systems made by several manufacturers have been recalled due to higher than normal rates of complications and premature implant failures.
DePuy Orthopaedics, which is a division of Johnson & Johnson, recalled its ASR Hip Resurfacing System and ASR XL Acetabular System. Two implant products made by Stryker Orthopaedics were recalled: the Rejuvenate and the ABG II modular-neck hip stems. Zimmer Holdings recalled its Durom Cup temporarily, returning it to the market with revised instructions, and Smith & Nephew recalled a component of its R3 Acetabular System.
Implant debris is the source of some of the more serious complications seen with these products, shed due to the friction between components as the patient walks. In the recalled replacement systems, design flaws and improper alignment of the components caused more wear and debris than is usual in hip implants, leading to high rates of debris-related complications and revision surgeries.
Among the most serious of these hip replacement complications is metallosis, which occurs when the soft tissues around the implant are contaminated with metallic debris particles. This can lead to severe pain and inflammation, tissue death, and bone death, often causing implant loosening and failure. In some cases, high levels of metal ions were also found to be circulating in the blood system, disbursed throughout the body. The long-term consequences of that widespread metal contamination in the body have yet to be determined. However, the U.S. Food and Drug Administration (FDA) states that metal ions in the blood can cause other symptoms or illnesses in the nervous system, thyroid gland and heart.
FDA Information and Recommendations
The FDA cautions that patients who have metal-on-metal hip replacements should watch for symptoms that include pain in the groin or leg, swelling at or near the hip joint and a limp or change in walking ability. If these symptoms emerge, patients should be thoroughly examined, and may need testing, including imaging tests, joint aspiration and blood tests to measure levels of metal ions in the blood. The agency also recommends that patients watch for general health symptoms, such as chest pain, shortness of breath, changes in vision or hearing, numbness or weakness, weight gain, fatigue and changes in urinary function.
Elizabeth Carrollton writes about defective medical devices and dangerous drugs for Drugwatch.com.
Posted by
Unknown
at
4:42 PM


Current Hip Replacement Issues
2012-10-04T16:42:00-04:00
Unknown
DePuy|Hip replacement surgery|implant failure|Johnson|Stryker|Zimmer|
Comments
Labels:
DePuy,
Hip replacement surgery,
implant failure,
Johnson,
Stryker,
Zimmer
Saturday, September 29, 2012
Price, not More Visits, Drives Cost Increases in Healthcare
Why should you care?
Commercial health care costs are going up - does it matter whether price or patient volume is to blame?
Yes. The Town Hall meeting at the recent Florida Physical Therapy Association (FPTA) meeting included discussion about Copayment reform legislation in Florida.
Some voices in the Town Hall argued that Copayment reform legislation in Florida is not necessary since rising physical therapy utilization indicates there are no barriers to patient access to physical therapists.
Increasing health care costs, to employers via premiums and to employees in the form of rising Copayments, reduce access to physical therapist services.
Do we want to live in an America where only the rich or the employed have access to physical therapist services?
The findings of the Health Care Cost Institute from September 2012 found that
According to a September 25th Washington Post article:
Other state physical therapy associations have not seen the same rapid success with Copayment reform. There is not even uniform agreement that Copayment reform is necessary for patients. Florida is one example where there is disagreement.
Some other opponents of Copayment reform at the recent Town Hall meeting in Daytona Beach spoke out and suggested that insurance companies would "get mad" at the FPTA if we, as an organization, supported Copayment reform.
These opponents, who are physical therapists, are supporting the insurance companies because the insurance companies support them.
When insurance companies set the political agenda for the FPTA we are allowing them to put profits before patients. We need Copayment reform to protect patients. From the Post article:
This problem wont go away and it can't be solved through "free market" methods.
States need legislative reform that lowers Copayments for patients.
Commercial health care costs are going up - does it matter whether price or patient volume is to blame?
Yes. The Town Hall meeting at the recent Florida Physical Therapy Association (FPTA) meeting included discussion about Copayment reform legislation in Florida.
Some voices in the Town Hall argued that Copayment reform legislation in Florida is not necessary since rising physical therapy utilization indicates there are no barriers to patient access to physical therapists.
Increasing health care costs, to employers via premiums and to employees in the form of rising Copayments, reduce access to physical therapist services.
Do we want to live in an America where only the rich or the employed have access to physical therapist services?
The findings of the Health Care Cost Institute from September 2012 found that
"... price growth for outpatient facilities and professional procedures remained higher than (patient volume) utilization growth.".The prices paid were the primary drivers of health care spending in 2011.
According to a September 25th Washington Post article:
"Employers typically have tried to control costs by reducing the volume of care delivered, whether that means higher co-pays for doctor visits or using prevention to catch costly diseases earlier."Copayment reform for physical therapy patients was a "slam dunk" in Kentucky, South Dakota and New Jersey in 2011 and 2012.
Other state physical therapy associations have not seen the same rapid success with Copayment reform. There is not even uniform agreement that Copayment reform is necessary for patients. Florida is one example where there is disagreement.
Some other opponents of Copayment reform at the recent Town Hall meeting in Daytona Beach spoke out and suggested that insurance companies would "get mad" at the FPTA if we, as an organization, supported Copayment reform.
These opponents, who are physical therapists, are supporting the insurance companies because the insurance companies support them.
When insurance companies set the political agenda for the FPTA we are allowing them to put profits before patients. We need Copayment reform to protect patients. From the Post article:
"Some economists have argued that government regulation is exactly what we need to slow price growth and ensure patient access.
Maryland is the only state in the USA where the government sets the rates that hospitals can charge insurance companies.
Maryland's hospitals from 1977 to 2009 experienced the lowest cumulative increase in cost per adjusted admission of any state in the nation. And private insurers pay the same rates as public insurers.
All states except Maryland gravitated away from those models, as states have looked for more competition and less regulation in health-care markets."Consumers will continue to need physical therapy services and employers will continue to buy lower priced health care with lower premiums for their employees. This means higher Copayments.
This problem wont go away and it can't be solved through "free market" methods.
States need legislative reform that lowers Copayments for patients.
Posted by
Unknown
at
8:45 AM


Price, not More Visits, Drives Cost Increases in Healthcare
2012-09-29T08:45:00-04:00
Unknown
Copayment reform|florida|florida physical therapy association|fpta|Health care costs|physical therapist|
Comments
Labels:
Copayment reform,
florida,
florida physical therapy association,
fpta,
Health care costs,
physical therapist
Monday, September 17, 2012
Are Physical Therapy Students Risk Averse?
Do physical therapy students always choose the safe alternative?
Does $100,000 in debt cause students to vote for the status quo?
Do physical therapists and students feel so much anxiety over health care reform that they prefer to vote for short-run self-interests over long-run investments?
Outcomes measurement linked to physical therapist reimbursement was the subject of the 2012 Oxford Debate at the Florida Physical Therapy Association Meeting (FPTA) in Daytona Beach. The students and physical therapists in the room - about 400 - mainly voted against using these measures for payment.
I question if students, in these changing times, are prepared to put the interests of their patients and their profession ahead of their own interests. I can't really blame them. I was a student once, too. The future is uncertain and scary.
This student-led decision was reminiscent of the American Physical Therapy Association's (APTA) 2011 Annual Conference in Washington DC when a student-dominated audience voted against Clinical Decision Rules.
Oxford Debates pit two teams arguing contrary positions. Each team "wins" by persuading the audience to cheer, make noise or physically move from one side of the room to the other. The side with the most supporters wins the debate. Most Oxford Debates handle serious topics in a fun environment. Drinks are usually served.
This convention was well-attended by students, many of them from the University of St. Augustine. The student-dominated audience split about 60/40 against using patient outcomes to reward physical therapists.
Inadequate risk adjustment seemed to be the main reason outcome measures should not be used, according to the speakers and the audience. In other words, the measure would ONLY capture the outcome of care which might depend on factors other than the therapists' effort and skill.
For instance, if the patient does not do their home exercise program they will tend to have worse outcomes than if they do their exercises. Older people with multiple diseases will usually have worse outcome scores at baseline and at follow-up than younger people without disease.
We've recently heard similar arguments in the Chicago teachers' strike when school teachers objected to being paid based on the standardized test scores (outcomes) of their students. The teachers argued that many factors that affect test scores are beyond their control. Paying teachers based on test scores was unfair since many of the determinants of teacher performance happened outside of the classroom.
A physical therapy student at the Oxford Debate noted that the most important determinants of health also occur outside the physical therapy clinic. These determinants are things like the following:
However, I think these students' behavior is rational.
Instead of pushing physical therapists and students to accept a reimbursement system that puts us at risk let's design a system that lets us think about patient care rather than worry about money.
What do you think?
Does $100,000 in debt cause students to vote for the status quo?
Do physical therapists and students feel so much anxiety over health care reform that they prefer to vote for short-run self-interests over long-run investments?
Outcomes measurement linked to physical therapist reimbursement was the subject of the 2012 Oxford Debate at the Florida Physical Therapy Association Meeting (FPTA) in Daytona Beach. The students and physical therapists in the room - about 400 - mainly voted against using these measures for payment.
I question if students, in these changing times, are prepared to put the interests of their patients and their profession ahead of their own interests. I can't really blame them. I was a student once, too. The future is uncertain and scary.
This student-led decision was reminiscent of the American Physical Therapy Association's (APTA) 2011 Annual Conference in Washington DC when a student-dominated audience voted against Clinical Decision Rules.
Oxford Debates pit two teams arguing contrary positions. Each team "wins" by persuading the audience to cheer, make noise or physically move from one side of the room to the other. The side with the most supporters wins the debate. Most Oxford Debates handle serious topics in a fun environment. Drinks are usually served.
This convention was well-attended by students, many of them from the University of St. Augustine. The student-dominated audience split about 60/40 against using patient outcomes to reward physical therapists.
Inadequate risk adjustment seemed to be the main reason outcome measures should not be used, according to the speakers and the audience. In other words, the measure would ONLY capture the outcome of care which might depend on factors other than the therapists' effort and skill.
For instance, if the patient does not do their home exercise program they will tend to have worse outcomes than if they do their exercises. Older people with multiple diseases will usually have worse outcome scores at baseline and at follow-up than younger people without disease.
We've recently heard similar arguments in the Chicago teachers' strike when school teachers objected to being paid based on the standardized test scores (outcomes) of their students. The teachers argued that many factors that affect test scores are beyond their control. Paying teachers based on test scores was unfair since many of the determinants of teacher performance happened outside of the classroom.
A physical therapy student at the Oxford Debate noted that the most important determinants of health also occur outside the physical therapy clinic. These determinants are things like the following:
- family and social support
- a positive outlook
- educational level
- addictive behaviors, such as cigarette smoking
- level of activity
However, I think these students' behavior is rational.
Instead of pushing physical therapists and students to accept a reimbursement system that puts us at risk let's design a system that lets us think about patient care rather than worry about money.
What do you think?
Posted by
Unknown
at
12:46 PM


Are Physical Therapy Students Risk Averse?
2012-09-17T12:46:00-04:00
Unknown
clinical decision rules|florida physical therapy association|fpta|outcome measures|Oxford Debate|physical therapist|physical therapy students|
Comments
Labels:
clinical decision rules,
florida physical therapy association,
fpta,
outcome measures,
Oxford Debate,
physical therapist,
physical therapy students
Friday, September 14, 2012
Exercise Prevents Falls in Older Adults but Cognitive Behavioral Therapy Does Not
Older adults falling down at home and elsewhere is a growing problem in the United States. About 30% of older people fall in a year.
An update of a 2009 Cochrane Review of the effectiveness of a falls reduction programs found that exercise and home safety interventions prevent falls in older adults.
The investigators assessed 159 randomized trials of fall prevention interventions with nearly 80,000 participants aged 60 and older.
Among the other interventions that helped reduce the rate of falls or risk for falls:
Some of the interventions that did not have an effect include:
An update of a 2009 Cochrane Review of the effectiveness of a falls reduction programs found that exercise and home safety interventions prevent falls in older adults.
The investigators assessed 159 randomized trials of fall prevention interventions with nearly 80,000 participants aged 60 and older.
Among the other interventions that helped reduce the rate of falls or risk for falls:
- Multifactorial interventions, including individualized risk assessment
- Tai chi
- Pacemakers, in patients with carotid sinus hypersensitivity
- First eye cataract surgery in women
- Gradual withdrawal of psychotropic drugs
- Changes in prescribing behavior by primary care physicians
- An anti-slip shoe device in icy conditions
Some of the interventions that did not have an effect include:
- Vitamin D supplementation in people with normal vitamin D levels
- Patient education alone
- Cognitive-behavioral therapy
Thursday, September 13, 2012
Town Hall Meeting Provokes Excitement
The Town Hall at 5:30pm on Thursday, September 13, 2012 at the FPTA Annual Conference & Assembly of Representatives in Daytona Beach was interesting, exiting and invigorating.
We heard many passionate, intelligent and involved physical therapists voicing their opinions.
The differences of opinion were sharp but friendly. The divide spun on the future direction of the FPTA advocacy resources.
In other words, we do have some political and social capital but which way do we spend it?
Tomorrow, I will present How to Open a Private Practice in Line with APTA's Vision 2020 with Adam Geril, DPT and Adam Woods, a banker.
My contribution will be Using Functional Outcome Questionnaires to Get Medicare Compliance.
I hope you can make it.
We heard many passionate, intelligent and involved physical therapists voicing their opinions.
The differences of opinion were sharp but friendly. The divide spun on the future direction of the FPTA advocacy resources.
In other words, we do have some political and social capital but which way do we spend it?
- Copayment legislation?
- Term Protection?
- PIP legislation?
Tomorrow, I will present How to Open a Private Practice in Line with APTA's Vision 2020 with Adam Geril, DPT and Adam Woods, a banker.
My contribution will be Using Functional Outcome Questionnaires to Get Medicare Compliance.
I hope you can make it.
Posted by
Unknown
at
11:32 PM


Town Hall Meeting Provokes Excitement
2012-09-13T23:32:00-04:00
Unknown
copayment legislation|fpta|medicare compliance|Outcome Questionnaires|physical therapists|private practice|
Comments
Labels:
copayment legislation,
fpta,
medicare compliance,
Outcome Questionnaires,
physical therapists,
private practice
Wednesday, September 12, 2012
Why We Have Brains
Neuroscientist Daniel Wopert suggests that human brains evolved for ONE REASON ONLY.
To control movement:
Not thinking, not reasoning, not tool-making.
Movement.
Dr. Wolpert's findings may have implications for physical therapists.
If our human brain needed to evolve in order to control movement, then restoration of movement may take priority over classic, medical approaches. The medical paradigm attempts to "cure" the patient or the pathology.
For example, spinal pain patients are often told that their bulging disc is the cause of their lower back pain. They may then be told that bending, lifting or twisting their back causes further disc bulging and pain. Their typical response is to further limit their activities, especially bending, lifting and twisting.
Perhaps movement therapy should begin before the "cure" or in place of the "cure".
Watch Dr. Wolpert's video and add your comments below this post. Thanks.
-->
To control movement:
Not thinking, not reasoning, not tool-making.
Movement.
Dr. Wolpert's findings may have implications for physical therapists.
If our human brain needed to evolve in order to control movement, then restoration of movement may take priority over classic, medical approaches. The medical paradigm attempts to "cure" the patient or the pathology.
For example, spinal pain patients are often told that their bulging disc is the cause of their lower back pain. They may then be told that bending, lifting or twisting their back causes further disc bulging and pain. Their typical response is to further limit their activities, especially bending, lifting and twisting.
Perhaps movement therapy should begin before the "cure" or in place of the "cure".
Watch Dr. Wolpert's video and add your comments below this post. Thanks.
Posted by
Unknown
at
1:18 PM


Why We Have Brains
2012-09-12T13:18:00-04:00
Unknown
Daniel Wopert|Lower Back Pain|physical therapists|
Comments
Labels:
Daniel Wopert,
Lower Back Pain,
physical therapists
Tuesday, September 11, 2012
Is there a physician shortage in America?
Uwe Reinhardt is an economics professor at Princeton and former keynote speaker at the American Physical Therapy Association (APTA) Annual Conference sometime back in the 1990's.
Professor Reinhardt pokes holes in the "doom-and-gloom" scenario of a pending physician shortage in America and I agree.
I wrote about this fallacy on November 28th, 2011 in Can Physical Therapists Replace Physicians as Primary Care Providers in Hospitals?
-->
I believe economic necessity will intervene as public policymakers and private payers join forces to push physical therapists into direct access roles for musculoskeletal conditions.
The time is right now. According to Professor Reinhardt:
Professor Reinhardt pokes holes in the "doom-and-gloom" scenario of a pending physician shortage in America and I agree.
I wrote about this fallacy on November 28th, 2011 in Can Physical Therapists Replace Physicians as Primary Care Providers in Hospitals?
I believe economic necessity will intervene as public policymakers and private payers join forces to push physical therapists into direct access roles for musculoskeletal conditions.
The time is right now. According to Professor Reinhardt:
"...the suspected physician shortage now imputed by critics of the Affordable Care Act may actually drive our health system into more efficient medical practice.
Step No. 1 in that direction, of course, would be to lighten the enormous administrative load now heaped by our health insurance system onto physicians devoted to rendering patient care."Delegating high-volume spinal pain, sports injuries and many chronic pain patients to physical therapists would relieve much of the physician workload and eliminate the physician shortage.
Posted by
Unknown
at
5:46 PM


Is there a physician shortage in America?
2012-09-11T17:46:00-04:00
Unknown
affordable care act|American Physical Therapy Association|APTA|direct access|physical therapists|Uwe Reinhardt|
Comments
Labels:
affordable care act,
American Physical Therapy Association,
APTA,
direct access,
physical therapists,
Uwe Reinhardt
Thursday, September 6, 2012
Taking Routine Blood Pressures in the Physical Therapy Clinic
Physical therapists should be taking routine blood pressures in the physical therapy clinic.
We have evidence that physical therapists don't routinely assess blood pressure from Jette and Jewell's April 2012 study in Physical Therapy Journal.
Only 11% of 2,544 physical therapists in all settings measured and followed-up with blood pressure. Every time your patient comes in you, or a member of your staff, should take and record their blood pressure.
The Centers' for Disease Control and Prevention (CDC) reported today that over one-half of American's have hypertension defined as
According to the CDC report: Vital Signs: Awareness and Treatment of Uncontrolled Hypertension Among Adults — United States, 2003–2010
Physical therapists can position themselves as primary care providers by providing increased blood pressure monitoring and referral. Primary care providers, physicians and otherwise, will be an important workforce component for hospital systems participating as Accountable Care Organizations (ACO) within the Medicare Shared Savings Program.
Finally, to prevent a Medicare Audit a physical therapist can document routine blood pressure measure before, during and after exercise can show Skilled Physical Therapy.
"Skilled Physical Therapy" means that your service normally wouldn't be provided by a lesser trained provider, such as a massage therapist or athletic trainer.
Physical therapists work on medically complex patients where safety is a key concern. We know that 7% to 12% of individuals experience an adverse response to exercise. Adverse response is defined as:
We have evidence that physical therapists don't routinely assess blood pressure from Jette and Jewell's April 2012 study in Physical Therapy Journal.
Only 11% of 2,544 physical therapists in all settings measured and followed-up with blood pressure. Every time your patient comes in you, or a member of your staff, should take and record their blood pressure.
The Centers' for Disease Control and Prevention (CDC) reported today that over one-half of American's have hypertension defined as
"...average systolic blood pressure (SBP) greater than 140 mmHg or an average diastolic blood pressure (DBP) greater than 90 mmHg, or currently using blood pressure (BP) lowering medication."Over one-third of Americans with hypertension were unaware of their problem and 90% of them had a usual source of care - that is, they had a doctor.
According to the CDC report: Vital Signs: Awareness and Treatment of Uncontrolled Hypertension Among Adults — United States, 2003–2010
"Nearly 90% of U.S. adults with uncontrolled hypertension have a usual source of health care and insurance, representing a missed opportunity for hypertension control.
Improved hypertension control will require an expanded effort and an increased focus on blood pressure from health-care systems, clinicians, and individuals."This is a major opportunity for physical therapists to assume an increased role in the care of Americans.
Physical therapists can position themselves as primary care providers by providing increased blood pressure monitoring and referral. Primary care providers, physicians and otherwise, will be an important workforce component for hospital systems participating as Accountable Care Organizations (ACO) within the Medicare Shared Savings Program.
Finally, to prevent a Medicare Audit a physical therapist can document routine blood pressure measure before, during and after exercise can show Skilled Physical Therapy.
"Skilled Physical Therapy" means that your service normally wouldn't be provided by a lesser trained provider, such as a massage therapist or athletic trainer.
Physical therapists work on medically complex patients where safety is a key concern. We know that 7% to 12% of individuals experience an adverse response to exercise. Adverse response is defined as:
"...an exercise-induced change that worsens a risk factor (such as BP) beyond measurement error and expected day-to-day variation."Physicians probably cannot detect these individuals reliably. Physical therapists could measure blood pressure changes during and after and on multiple sessions of exercise. Adverse changes could provide the physical therapist with cues that could indicate a change in the Plan of Care or referral.
Posted by
Unknown
at
1:39 PM


Taking Routine Blood Pressures in the Physical Therapy Clinic
2012-09-06T13:39:00-04:00
Unknown
ACCOUNTABLE CARE ORGANIZATIONS|aco|blood pressure|hypertension|Medicare audit|physical therapy|primary care providers|skilled physical therapy|
Comments
Labels:
ACCOUNTABLE CARE ORGANIZATIONS,
aco,
blood pressure,
hypertension,
Medicare audit,
physical therapy,
primary care providers,
skilled physical therapy
Tuesday, August 28, 2012
Dear Tim, I need your help...
Dear Tim,
I need your help.
We are trying to spread the word about Medifest Jacksonville on September 12-13. Could you please forward the email below to your contacts? I appreciate your help!
Registration will be open until Wednesday, September 5 close of business.
First Coast Service Options (FCSO), your Medicare contractor in Florida, invites you to register today for our premiere Medicare educational conference, Medifest, on September 12-13, 2012, at the Jacksonville Marriot in Jacksonville, FL.
Medifest brings together Medicare experts, providers, and vendors to learn about what's trending now in Medicare and how to lower your risk of payment recoupment and claim submission errors through improved billing practices.
We are excited to return to Jacksonville this year, and it is a direct result of your feedback! This year's event offers 24 data-driven workshops and seminars geared to the needs of our providers in northeast Florida.
Our classes include:
Click here for a full list of course schedules.
Get the Medifest 2012 Jacksonville brochure to learn more about Medifest, including registration fees, review ourbrochure.
Register today: Register for Medifest through your account at FCSO'straining website and select the "Medifest" page.
Don't have an account? No worries. Providers can request a free account today by visiting the site and selecting "Request a New Account" in the Login section.
Once you request an account, we will send you an email within a few days with the temporary password.
Our goal is to build a stronger Medicare community through education, so please join us for just one day or both!
Thanks!
Julie Stiles
Training Administrator First Coast Service Options, Inc.
When Experience Counts and Quality Matters
I need your help.
We are trying to spread the word about Medifest Jacksonville on September 12-13. Could you please forward the email below to your contacts? I appreciate your help!
Registration will be open until Wednesday, September 5 close of business.
First Coast Service Options (FCSO), your Medicare contractor in Florida, invites you to register today for our premiere Medicare educational conference, Medifest, on September 12-13, 2012, at the Jacksonville Marriot in Jacksonville, FL.
Medifest brings together Medicare experts, providers, and vendors to learn about what's trending now in Medicare and how to lower your risk of payment recoupment and claim submission errors through improved billing practices.
We are excited to return to Jacksonville this year, and it is a direct result of your feedback! This year's event offers 24 data-driven workshops and seminars geared to the needs of our providers in northeast Florida.
Our classes include:
- Provider Enrollment and PECOs web
- Avoiding roadblocks in billing Medicare secondary payer
- Learning about First Coast's exclusive online provider resources on our education and training websites
- Improving compliance with medical documentation requirements
- Applying correctly global surgery modifiers
- Learning the "ins and outs" of billing cost outlier claims (Part A)
- Selecting the proper evaluation and management code
- Understanding the Medicare appeals process
- ICD-10 transition
- Claims resources and resolutions, and much more!
Click here for a full list of course schedules.
Get the Medifest 2012 Jacksonville brochure to learn more about Medifest, including registration fees, review ourbrochure.
Register today: Register for Medifest through your account at FCSO'straining website and select the "Medifest" page.
Don't have an account? No worries. Providers can request a free account today by visiting the site and selecting "Request a New Account" in the Login section.
Once you request an account, we will send you an email within a few days with the temporary password.
Our goal is to build a stronger Medicare community through education, so please join us for just one day or both!
Thanks!
Julie Stiles
Training Administrator First Coast Service Options, Inc.
When Experience Counts and Quality Matters
Thursday, August 23, 2012
Tim Richardson Running for Secretary of the Florida Physical Therapy Association
Statement: I would be honored to serve my fellow physical therapists as Secretary of the Board of Directors of the Florida Physical Therapy Association (FPTA).
The FPTA Board of Directors is a responsibility I take very seriously since the FPTA is the largest organization representing physical therapists and physical therapist assistants in the State of Florida.
I believe our voice is strongest when we speak, not from our own self-interest, but from the perspective of our patients. I believe we should ask ourselves, when developing FPTA policy:
During the FPTA Annual Conference in Orlando, candidates will have the opportunity to speak during the Chapter Caucus. Additionally, the Nominating Committee has scheduled a "Meet the Candidates: session during the Exhibit Reception. Members will have the opportunity to chat with candidates and ask any questions they feel necessary.
Biography: Tim Richardson graduated from the University of Florida in 1992 with a Bachelor's in Health Science (Physical Therapy).
Tim received Manual Therapy Certification from the University of St. Augustine in 2001. Since 1996 he has owned and managed private physical therapy clinics in Manatee County, Florida.
Tim is returning from a one-year sabbatical in Spain where he provided cash-based musculoskeletal and vestibular physical therapy services to Spanish-speaking people.
Tim just recently (June 2012) was elected to the North Central Florida Health Information Management Systems Society (HiMSS) Health Information Exchange Committee, which advises the HiMSS Board of Directors.
He is also a founding member of the Florida Physical Therapists in Private Practice (FLPTPP), serves on their Board of Directors and serves as their Legislative Chair.
Tim is serving his third year on the Florida Physical Therapy Association (FPTA) Government Affairs Committee and has served on the Web Site Task Force responsible for the FPTA logo. Tim also serves on the American Physical Therapy Association (APTA) Orthopedic Section Practice Committee and the Health Policy & Admin Section Technology Special Interest Group.
Tim advises the Florida Medicare Administrative Contractor, First Coast Service Options Inc., as a member of the Provider Outreach and Education Advisory Group.
Contact Information:
email: TimRichPT@MedicalArtsRehab.com
LinkedIn profile: http://linkd.in/zPc0EH
Twitter handle: https://twitter.com/#!/timrichpt
Skype name: TimRichPT
Facebook: http://www.facebook.com/timrichpt
Thank you for your consideration.
Remember, in a democracy its not "Majority Rules", but the majority of people WHO VOTE that make the rules.
The FPTA Board of Directors is a responsibility I take very seriously since the FPTA is the largest organization representing physical therapists and physical therapist assistants in the State of Florida.
I believe our voice is strongest when we speak, not from our own self-interest, but from the perspective of our patients. I believe we should ask ourselves, when developing FPTA policy:
"What can I do, as an FPTA member, that can improve my ability to provide care or the ability of my patients to access my services?"
***
Online voting for FPTA offices began on Tuesday, August 14 at 9:00 am and will close on Friday, September 14 at 8:30 pm. FPTA will use the emails on file with APTA for contacting members regarding elections and voting procedures.
During the FPTA Annual Conference in Orlando, candidates will have the opportunity to speak during the Chapter Caucus. Additionally, the Nominating Committee has scheduled a "Meet the Candidates: session during the Exhibit Reception. Members will have the opportunity to chat with candidates and ask any questions they feel necessary.
Biography: Tim Richardson graduated from the University of Florida in 1992 with a Bachelor's in Health Science (Physical Therapy).
Tim received Manual Therapy Certification from the University of St. Augustine in 2001. Since 1996 he has owned and managed private physical therapy clinics in Manatee County, Florida.
Tim is returning from a one-year sabbatical in Spain where he provided cash-based musculoskeletal and vestibular physical therapy services to Spanish-speaking people.
Tim just recently (June 2012) was elected to the North Central Florida Health Information Management Systems Society (HiMSS) Health Information Exchange Committee, which advises the HiMSS Board of Directors.
He is also a founding member of the Florida Physical Therapists in Private Practice (FLPTPP), serves on their Board of Directors and serves as their Legislative Chair.
Tim is serving his third year on the Florida Physical Therapy Association (FPTA) Government Affairs Committee and has served on the Web Site Task Force responsible for the FPTA logo. Tim also serves on the American Physical Therapy Association (APTA) Orthopedic Section Practice Committee and the Health Policy & Admin Section Technology Special Interest Group.
Tim advises the Florida Medicare Administrative Contractor, First Coast Service Options Inc., as a member of the Provider Outreach and Education Advisory Group.
Contact Information:
email: TimRichPT@MedicalArtsRehab.com
LinkedIn profile: http://linkd.in/zPc0EH
Twitter handle: https://twitter.com/#!/timrichpt
Skype name: TimRichPT
Facebook: http://www.facebook.com/timrichpt
Thank you for your consideration.
Remember, in a democracy its not "Majority Rules", but the majority of people WHO VOTE that make the rules.
Posted by
Unknown
at
5:48 AM


Tim Richardson Running for Secretary of the Florida Physical Therapy Association
2012-08-23T05:48:00-04:00
Unknown
Board of Directors|Florida Physical Therapists in Private Practice|florida physical therapy association|flptpp|fpta|
Comments
Labels:
Board of Directors,
Florida Physical Therapists in Private Practice,
florida physical therapy association,
flptpp,
fpta
Friday, August 17, 2012
Legislative Meeting Kicks Off FLPTPP 2012
The Florida Physical Therapists' in Private Practice (FLPTPP) Legislative Committee Meeting kicks off the 2nd Annual FLPTPP Conference today, August 17th, 2012, at the:
The FLPTPP is hosting Phil Moe, South Dakota's Chief Delegate and Board of Directors' member.
As many readers of this blog are aware, South Dakota is one of three states that have recently enacted patient protection legislation to prevent insurance companies from charging patients excessively high copayments for physical therapy.
Phil will describe the legislative strategy his state association used to achieve their legislative success. The meeting starts at 5pm in the Hilton Palm 3 conference room.
On-site registration for the conference is available.
Hilton Orlando Resort, Lake Buena Vista 1751, Hotel Plaza Blvd, Lake Buena Vista, Florida
 |
| I-4 corridor to the FLPTPP meeting in Orlando |
As many readers of this blog are aware, South Dakota is one of three states that have recently enacted patient protection legislation to prevent insurance companies from charging patients excessively high copayments for physical therapy.
Phil will describe the legislative strategy his state association used to achieve their legislative success. The meeting starts at 5pm in the Hilton Palm 3 conference room.
On-site registration for the conference is available.
Posted by
Unknown
at
1:42 PM


Legislative Meeting Kicks Off FLPTPP 2012
2012-08-17T13:42:00-04:00
Unknown
Florida Physical Therapists' in Private Practice|flptpp|high copayments|physical therapy|south dakota|
Comments
Labels:
Florida Physical Therapists' in Private Practice,
flptpp,
high copayments,
physical therapy,
south dakota
Monday, August 13, 2012
Picking Physical Therapists' Pockets...
Physical therapists in private practice (and other settings) should understand where most our dollars come from.
In Florida, with our large elderly population, about half of my practice income is Medicare reimbursement.
That reimbursement is getting smaller - not due to budget cuts - but due to the activities of specialist physicians.
We haven't had an actual Medicare reimbursement cut since 2002.
Despite the media hoopla about the effect of the (Un)Sustainable Growth Rate on the Medicare Physicians' Fee Schedule, the Congress of the United States has failed to implement budget balancing reforms on Medicare reimbursement.
So why has my relative income continued to decline?
The Relative value Update Committee (RUC) of the American Medical Association each year recommends changes to Medicare reimbursements that reward specialty physicians yet penalize general medicine and preventative services.
Specialists are picking physical therapists' pocket and most physical therapists don't even know it!
The media and our own professional political advocacy would have us focus most of our attention on the SGR. However, the RUC is, according to Dr. Brian Klepper...
Dr. Klepper has also formed the advocacy group called Replace the RUC to generate public awareness of this shadowy politcal group.
Who thinks physical therapy codes are under-valued relative to certain other medical procedures?
Which codes? Which procedures?
Thanks for commenting.
In Florida, with our large elderly population, about half of my practice income is Medicare reimbursement.
That reimbursement is getting smaller - not due to budget cuts - but due to the activities of specialist physicians.
We haven't had an actual Medicare reimbursement cut since 2002.
Despite the media hoopla about the effect of the (Un)Sustainable Growth Rate on the Medicare Physicians' Fee Schedule, the Congress of the United States has failed to implement budget balancing reforms on Medicare reimbursement.
| Year | Projected Update to the SGR | Actual Update to the SGR |
| 2002 | -4.8% | -4.8 |
| 2003 | -4.4% | 1.4% |
| 2004 | -4.5% | 1.5% |
| 2005 | -3.3% | 1.5% |
| 2006 | -4.4% | 0.2% |
| 2007 | -5.0% | 0% |
| 2008 | -10.1% | 0.5% |
| 2009 | -10.6% | 1.1% |
| 2010 | -21.3% | 0% |
| 2011 | -27.4% | 0% |
So why has my relative income continued to decline?
The Relative value Update Committee (RUC) of the American Medical Association each year recommends changes to Medicare reimbursements that reward specialty physicians yet penalize general medicine and preventative services.
Specialists are picking physical therapists' pocket and most physical therapists don't even know it!
The media and our own professional political advocacy would have us focus most of our attention on the SGR. However, the RUC is, according to Dr. Brian Klepper...
"...the greatest obstacle to turning around our healthcare system and our economy."Dr. Klepper details the scope and scale of this problem in his August 2012 blogpost The Most Powerful Health Care Group You’ve Never Heard Of
Dr. Klepper has also formed the advocacy group called Replace the RUC to generate public awareness of this shadowy politcal group.
Who thinks physical therapy codes are under-valued relative to certain other medical procedures?
Which codes? Which procedures?
Thanks for commenting.
Posted by
Unknown
at
7:39 AM


Picking Physical Therapists' Pockets...
2012-08-13T07:39:00-04:00
Unknown
Medicare Physicians' Fee Schedule|medicare reimbursement|Physical therapists in private practice|reimbursement|Relative Value Update Committee|
Comments
Labels:
Medicare Physicians' Fee Schedule,
medicare reimbursement,
Physical therapists in private practice,
reimbursement,
Relative Value Update Committee
Friday, August 10, 2012
Physical Therapy and Health Information Technology
Why Physical Therapists Should Make Diagnoses
"Physical therapy is not a subspecialty of the medical profession and physical therapists are not medical doctors; we are a separate profession that provides a unique service that physicians are unable and untrained to provide."
Letter to the American Medical Association from John Barnes
CEO, American Physical Therapy Association
12/22/2009
Letter to the American Medical Association from John Barnes
CEO, American Physical Therapy Association
12/22/2009
Posted by
Unknown
at
6:03 AM


Why Physical Therapists Should Make Diagnoses
2012-08-10T06:03:00-04:00
Unknown
American Medical Association|American Physical Therapy Association|physical therapy|physicians|
Comments
Labels:
American Medical Association,
American Physical Therapy Association,
physical therapy,
physicians
Private Practice Physical Therapists' Continuing Education
Click the image to get continuing education for Private Practice Physical Therapists:
See you in Orlando!
See you in Orlando!
Saturday, August 4, 2012
Free Giveaways at 2012 Florida Private Practice Conference
Tuesday, July 31, 2012
The Surprising Truth About Healthcare Fraud
Posted by
Unknown
at
3:25 PM


The Surprising Truth About Healthcare Fraud
2012-07-31T15:25:00-04:00
Unknown
health care|healthcare fraud|
Comments
Labels:
health care,
healthcare fraud
British Physical Therapists Gain Prescribing Rights
"This is a truly historic day..."The 51,000 British physical therapists (physiotherapists) can now become trained to independently prescribe medications to their patients.
They are the world's first physical therapists to be granted drug prescribing rights within their health care systems without needing a physician to sign the prescription.
"Once suitably trained, physiotherapists in the United Kingdom will be the first in the world to be able to independently prescribe medicines where clinically appropriate,such as painkillers and anti-inflammatories", said Earl Howe, the British Department of Health’s Under Secretary for Quality.The decision would reduce a layer of bureaucracy and an unnecessary burden on doctors who have, until now, had to counter-sign prescriptions drawn up by physiotherapists who have been "supplementary prescribers" since 2006.
The response from the British medical profession has been overwhelmingly positive.
British physical therapists fought for 10 years to gain independent prescription rights.
I would like to see the same changes take place in the United States of America, however, I am doubtful that the American medical establishment would be as supportive of physical therapists as the British physicians seem to be.
Evidence that increased competition (possibly from physical therapists) drives down prices and increases quality of American healthcare would only be seen as reducing physician income.
Fear of lower physician salaries would draw political opposition from the American Medical Association.
Presumably, Great Britain's "administered price system" (similar to Medicare) is what allows physicians to support physical therapist prescription rights.
What do you think?
Friday, July 20, 2012
Marcus Welby is Dead
"It's the death knoll of the private practice..." said Kurt Mosley, vice president of strategic lliances for Merritt Hawkins and Staff Care, a nationwide healthcare staffing organization.
"...I think... nobody wants Marcus Welby any more."
"That concept doesn’t play anymore and it’s not effective."Recruitment of physicians into private practice is now only 1% of all physician recruitment activities.
"It’s not necessarily that surprising, but it dropped so dramatically (this year)."This article from Healthcare Finance News sources Mosley's statement and provides additional links to explore these changes in physician recruitment.
Marcus Welby, MD delt with sensitive medical issues, such as depression, brain damage, breast cancer, sexually transmitted diseases, epilepsy, leukemia and Alzheimer's Disease.
How Do Physician Employment Trends Impact Outpatient Physical Therapists?
Fundamentally, physical therapists' practice and physicians' practice are different.
Physicians require access to sophisticated testing, technology and the resources of the acute care hospital to practice effectively in these medern times.
Physical therapists may also need access to hospitals, but to a lesser extent than physicians (which helps explain why physical therapists are not included in Meaningful Use incentive payments for providers who purchase Electronic Medical Records and achieve interoperability with hospitals).
This American Physical Therapy Association (APTA) letter to the American Medical Association (AMA) nails the point, exactly:
"Doctors of physical therapy are not medical doctors, and medical doctors are not doctors of physical therapy.
Physical therapy is not a subspecialty of the medical profession.
Physical therapists provide a unique but complimentary service that physicians are untrained to provide."Trends affecting medical doctors could buffet private practice physical therapists but seem unlikely to put the nail in the coffin of private practice physical therapists the way some are predicting for medical doctors.
I think the future is bright for private practice physical therapists. Its not a future like those who went before us, like Marcus Welby.
It could be better.
Posted by
Unknown
at
6:03 PM


Marcus Welby is Dead
2012-07-20T18:03:00-04:00
Unknown
Doctors of physical therapy|Marcus Welby|Outpatient Physical Therapists|physical therapists|physicians|private practice|
Comments
Labels:
Doctors of physical therapy,
Marcus Welby,
Outpatient Physical Therapists,
physical therapists,
physicians,
private practice
Tuesday, July 17, 2012
How to Tell Your Patient Their MRI is Unneccesary
Thanks to EIM faculty member Dr. Jason R. Rodeghero for this fun, thought-provoking video.
Physical therapists can educate their patients on the potential harm from excessive MRI imaging (and x-ray imaging).
I'm still amazed when I talk to my peers who accept "what the doctor ordered" just because the physician ordered it.
Physical therapy is a doctoring profession because we accept responsibility for our patients.
That includes pointing out to them when we believe unnecessary testing could harm them.
Physical therapists can educate their patients on the potential harm from excessive MRI imaging (and x-ray imaging).
I'm still amazed when I talk to my peers who accept "what the doctor ordered" just because the physician ordered it.
Physical therapy is a doctoring profession because we accept responsibility for our patients.
That includes pointing out to them when we believe unnecessary testing could harm them.
Posted by
Unknown
at
12:07 PM


How to Tell Your Patient Their MRI is Unneccesary
2012-07-17T12:07:00-04:00
Unknown
excessive imaging|physical therapists|x-ray|
Comments
Labels:
excessive imaging,
physical therapists,
x-ray
Monday, July 16, 2012
How to Open a Private Practice in line with APTA's Vision 2020
Intended for Physical Therapists new to Private Practice!
This course presents an introduction for healthcare professionals looking to open a private practice for the first time.
Specifically, this course will review reasons for opening a private practice, how to assess the market to determine potential success. This course will also review financing options, as well as how to monitor success by identifying critical metrics specific to your practice setting.
This course will expose the participant in how to develop a marketing plan.
Lastly, this course will review appropriate billing practices and how to document medical necessity and skilled Physical Therapy need to insure prompt and correct payments to facilitate on going cash flow to run your business.
Friday September 14th from 8am to 12pm at the FPTA Annual conference in Orlando.
Sign up here!
This course presents an introduction for healthcare professionals looking to open a private practice for the first time.
Specifically, this course will review reasons for opening a private practice, how to assess the market to determine potential success. This course will also review financing options, as well as how to monitor success by identifying critical metrics specific to your practice setting.
This course will expose the participant in how to develop a marketing plan.
Lastly, this course will review appropriate billing practices and how to document medical necessity and skilled Physical Therapy need to insure prompt and correct payments to facilitate on going cash flow to run your business.
Friday September 14th from 8am to 12pm at the FPTA Annual conference in Orlando.
Sign up here!
- Adam C. Geril, PT, DPT, MS, OCS, ATC
- Tim Richardson, PT
- Adam Woods, VP Alarion Bank
Posted by
Unknown
at
7:08 AM


How to Open a Private Practice in line with APTA's Vision 2020
2012-07-16T07:08:00-04:00
Unknown
fpta|FPTA Annual conference|New Graduate Physical Therapists|physical therapists|private practice|
Comments
Labels:
fpta,
FPTA Annual conference,
New Graduate Physical Therapists,
physical therapists,
private practice
Tuesday, July 10, 2012
Florida Physical Therapists Wanted to Speak to Legislators
The Key Contacts program of the Florida Physical Therapy Association (FPTA) is designed to put a physical therapist (PT) or physical therapist assistant (PTA) in every state legislator's office in Florida.
Each Florida legislator has an office in your district. Maybe your legislator has an office in your town.
We especially need therapists in the South Florida area.
The goal is to make politics personal so when the FPTA has an issue that needs support - such as the recently successful Temporary Licensure law - then we can reach out to the legislator.
But we need you to make that face-to-face contact.
The Florida Physical Therapy Association will be making strategic contributions to several legislators in anticipation of the 2013 legislative cycle.
You can set up a Practice Visit to meet you, your staff and your patients.
The FPTA may want to suport your legislator using FPTA Political Action Committee (PAC) funds.
Find out if your legislator in on the list by e-mailing Eric Chaconas, DPT.
Each Florida legislator has an office in your district. Maybe your legislator has an office in your town.
We especially need therapists in the South Florida area.
The goal is to make politics personal so when the FPTA has an issue that needs support - such as the recently successful Temporary Licensure law - then we can reach out to the legislator.
But we need you to make that face-to-face contact.
The Florida Physical Therapy Association will be making strategic contributions to several legislators in anticipation of the 2013 legislative cycle.
You can set up a Practice Visit to meet you, your staff and your patients.
The FPTA may want to suport your legislator using FPTA Political Action Committee (PAC) funds.
Find out if your legislator in on the list by e-mailing Eric Chaconas, DPT.
Posted by
Unknown
at
11:03 AM


Florida Physical Therapists Wanted to Speak to Legislators
2012-07-10T11:03:00-04:00
Unknown
florida physical therapy association|fpta|key contacts|physical therapy|Temporary Licensure|
Comments
Labels:
florida physical therapy association,
fpta,
key contacts,
physical therapy,
Temporary Licensure
Saturday, July 7, 2012
Physical Therapists Learn from the Best in the Business
Physical therapists learning from each other - that's what we've always done.
The 2012 Florida Physical Therapists in Private Practice (FLPTPP) Meeting is August 17th to 19th, 2012 in Orlando, Florida.
Armin Loges, PT and crew have lined up a dynamite cast of presenters for you.
Pick the educational courses that you need this year - all come with CME credits!
Last year's conference was important just because of the energy in the room and the excitement it generated (as well as the MANY new members of the FLPTPP that joined!)
This year's conference promises to be MUCH bigger, MUCH better and MUCH more exciting.
We'll see you there!
Sign up here!
The 2012 Florida Physical Therapists in Private Practice (FLPTPP) Meeting is August 17th to 19th, 2012 in Orlando, Florida.
Armin Loges, PT and crew have lined up a dynamite cast of presenters for you.
 |
| Florida Physical Therapists in Private Practice 2012 Annual Meeting |
| Saturday, August 18th (morning) | Medicare Compliance | Nancy Beckley, MS, MBA, CHC |
| Saturday, August 18th (morning) | Pelvic Floor Dysfunction | Tricia Trinque, MHE, PT |
| Saturday, August 18th (morning) | Dry Needling | Brian Ruchin, PT, DPT |
| Saturday, August 18th (afternoon) | Marketing Your PT Practice | Nitin Chhoda, DPT |
| Saturday, August 18th (afternoon) | Cervical Thrust Manipulation | James Dunning, FAAOMPT, MMACP |
| Saturday, August 18th (afternoon) | Business 101 for Physical Therapists | Dick Hillyer, DPT, MBA, MSM |
| Saturday, August 18th (afternoon) | Innovation in Physical Therapy | Matthew Harkness, MPT, MTC, TATC, CEAS |
| Sunday, August 19th (morning) | New Florida PIP law | Dick Hillyer, DPT, MBA |
| Sunday, August 19th (morning) | Red Flags for Cervical Instability | Eric Douglass, DPT, OCS, FAAOMPT |
| Sunday, August 19th (morning) | Legal Implications for Physical Therapists | Michael Magidson, Esq. |
| Sunday, August 19th (morning) | Acupuncture | Irene Hujsa, PT, OCS and Julietta Planchart, PT, CNS |
| Sunday, August 19th (afternoon) | DME and PTPP | Timothy Beury |
Last year's conference was important just because of the energy in the room and the excitement it generated (as well as the MANY new members of the FLPTPP that joined!)
This year's conference promises to be MUCH bigger, MUCH better and MUCH more exciting.
We'll see you there!
Sign up here!
Thursday, June 21, 2012
Is the Severity-Intensity Model a Roadmap for Fraud and Abuse?
First, I'd like to thank all the hard-working staff and volunteers at the American Physical Therapy Association (APTA) for the effort that went into developing the Severity-Intensity Model, also known as the Alternative Payment System (APS).
Like them, I'd like to see payment reform. But, I want reform that preserves the autonomy of the therapist-patient collaboration rather than depends on centralized oversight of physical therapists by government regulators.
I'm afraid the Severity-Intensity Model may just increase the ability of regulators to audit physical therapists.
Physical therapists are set-up to fail, in every setting, by a documentation framework that was never intended to capture the patient experience of chronically disabled adults.
The Physical Therapy Business Alliance keyed-in on a central flaw in Severity-Intensity in its post at EIM on June 13th, 2012:
Severity-Intensity Would Increase "Fraudbusting", not fraud
This chart is derived from the Development Draft for APTA Members: An Alternative Payment System for Physical Therapy Services - APTA members have until Friday, June 22nd to comment.
Go to this link and add your two cents.
The yellow cells are 1-on-1 codes that require individualized interaction between the qualified healthcare professional and the patient.
We all think OUR patients are more difficult to treat than our fellow therapists' patients - this is true in medicine too and is known as Response Bias (seeing what you expect to find). Therefore, using Severity-Intensity we would expect to see a "southeast shift" in coding based on this chart - every patient belongs in the yellow highlighted cells.
"Code inflation" would occur, based on coding and reimbusement seminars promoted by "Medicare Experts" - here's an example I received yesterday in my e-mail:
Is this what we want Doctors of Physical Therapy spending their time on in the 21st century? Writing this blah-blah-blah?
I think your time, and mine, is more valuable than that.
And, technology is increasingly bringing us better documentation alternatives.
Severity-Intensity just adds a layer of complexity on top of the flawed documentation framework that wastes so much time and physical therapist productivity.
What Now?
The Severity-Intensity Model needs to be accepted by the American Medical Association Relative Value Update Committee (AMA RUC) which may then recommend Severity-Intensity to the Centers for Medicare and Medicaid Services (CMS) to be used within its Current Procedure Terminology (CPT) Healthcare Common Procedure Coding System (HCPCS) IN PLACE OF the CPT 92505-97799 codes (also a few G-codes and a few others, possibly).
What Do We Use Instead of Severity-Intensity?
The American Academy of Family Physicians (AAFP) has proposed to the Congress a primary care-based Medical Home Model which pays primary care physicians three ways:
Like them, I'd like to see payment reform. But, I want reform that preserves the autonomy of the therapist-patient collaboration rather than depends on centralized oversight of physical therapists by government regulators.
I'm afraid the Severity-Intensity Model may just increase the ability of regulators to audit physical therapists.
Physical therapists are set-up to fail, in every setting, by a documentation framework that was never intended to capture the patient experience of chronically disabled adults.
The Physical Therapy Business Alliance keyed-in on a central flaw in Severity-Intensity in its post at EIM on June 13th, 2012:
"However, the APS in its current form disproportionately emphasizes administrative and regulatory requirements (ie, documentation, compliance, etc.) at the expense of the most critical elements of the clinical encounter, which is incentivizing quality clinical outcomes and patient satisfaction."We're not alone - this telling indicator of professional consensus is the OVERWHELMINGLY NEGATIVE comments posted at the PTinMotion web site in response to an article on the Severity-Intensity model.
Severity-Intensity Would Increase "Fraudbusting", not fraud
This chart is derived from the Development Draft for APTA Members: An Alternative Payment System for Physical Therapy Services - APTA members have until Friday, June 22nd to comment.
Go to this link and add your two cents.
| Recommended Times for Severity-Intensity Patient Visits | |||
| Patient Severity at the time of the Visit | |||
| Intensity of Therapist Decision Making | Limited | Moderate | Significant |
| Limited | 30 minutes | 30 minutes | 30 minutes |
| Moderate | 31 - 45 minutes | 31 - 45 minutes | 31 - 45 minutes |
| Significant | 45 minutes | 45 minutes | 45 minutes |
The yellow cells are 1-on-1 codes that require individualized interaction between the qualified healthcare professional and the patient.
We all think OUR patients are more difficult to treat than our fellow therapists' patients - this is true in medicine too and is known as Response Bias (seeing what you expect to find). Therefore, using Severity-Intensity we would expect to see a "southeast shift" in coding based on this chart - every patient belongs in the yellow highlighted cells.
"Code inflation" would occur, based on coding and reimbusement seminars promoted by "Medicare Experts" - here's an example I received yesterday in my e-mail:
"Treatment consists of manual therapy, 97140, to reduce swelling and scar formation followed by passive, active assistive ROM exercise to improve ROM at the knee; 97110, quad sets, SAQ, and SLR to promote the efficiency of the quad contraction and promote quad control at the knee joint, 97112; and finally, I want to put it all together by working on sit to stand transfers emphasizing knee flexion in sitting and equal weight distribution in sit to stand and stand to sit, 97530."Really?
Is this what we want Doctors of Physical Therapy spending their time on in the 21st century? Writing this blah-blah-blah?
I think your time, and mine, is more valuable than that.
And, technology is increasingly bringing us better documentation alternatives.
Severity-Intensity just adds a layer of complexity on top of the flawed documentation framework that wastes so much time and physical therapist productivity.
What Now?
The Severity-Intensity Model needs to be accepted by the American Medical Association Relative Value Update Committee (AMA RUC) which may then recommend Severity-Intensity to the Centers for Medicare and Medicaid Services (CMS) to be used within its Current Procedure Terminology (CPT) Healthcare Common Procedure Coding System (HCPCS) IN PLACE OF the CPT 92505-97799 codes (also a few G-codes and a few others, possibly).
What Do We Use Instead of Severity-Intensity?
The American Academy of Family Physicians (AAFP) has proposed to the Congress a primary care-based Medical Home Model which pays primary care physicians three ways:
- Fee for Service for each individual procedure
- a care management fee that compensates for expertise and time such as management and care coordination that are not direct patient encounters
- Pay for performance based on hitting benchmarked process and outcome measures
Posted by
Unknown
at
5:43 PM


Is the Severity-Intensity Model a Roadmap for Fraud and Abuse?
2012-06-21T17:43:00-04:00
Unknown
AMA RUC|American Medical Association|American Physical Therapy Association|APTA|cms|Current Procedure Terminology|Medical Home|Medicare|Relative Value Update Committee|Severity-Intensity Model|
Comments
Labels:
AMA RUC,
American Medical Association,
American Physical Therapy Association,
APTA,
cms,
Current Procedure Terminology,
Medical Home,
Medicare,
Relative Value Update Committee,
Severity-Intensity Model
Monday, June 18, 2012
Physical Therapists Cannot Opt-Out of Medicare
From First Coast Service Options e-news (June 18th, 2012): Private contracts between beneficiaries and physicians or practitioners.
Title 42, Part 405 of the Code of Federal Regulations outlines the guidelines and requirements for physicians and/or non-physician practitioners who wish to enter into private contracts (opt out).
These regulations permit a physician or practitioner to opt out of Medicare and enter into private contracts with Medicare beneficiaries, if specific requirements of these instructions are met.
Definition of physician or practitioner
For purposes of this provision, the term “physician” is limited to doctors of medicine and doctors of osteopathy who are legally authorized to practice medicine and surgery by the state in which such function or action is performed; no other physicians may opt out.
Also, for purposes of this provision, the term “practitioner” means any of the following to the extent that they are legally authorized to practice by the State and otherwise meet Medicare requirements:
The opt-out law does not define “physician” to include chiropractors; therefore, they may not opt out of Medicare and provide services under private contract.
Physical therapists in independent practice and occupational therapists in independent practice cannot opt out because they are not within the opt-out law’s definition of either a “physician” or “practitioner.”
Title 42, Part 405 of the Code of Federal Regulations outlines the guidelines and requirements for physicians and/or non-physician practitioners who wish to enter into private contracts (opt out).
These regulations permit a physician or practitioner to opt out of Medicare and enter into private contracts with Medicare beneficiaries, if specific requirements of these instructions are met.
Definition of physician or practitioner
For purposes of this provision, the term “physician” is limited to doctors of medicine and doctors of osteopathy who are legally authorized to practice medicine and surgery by the state in which such function or action is performed; no other physicians may opt out.
Also, for purposes of this provision, the term “practitioner” means any of the following to the extent that they are legally authorized to practice by the State and otherwise meet Medicare requirements:
- Physician assistant
- Nurse practitioner
- Clinical nurse specialist
- Certified registered nurse anesthetist
- Certified nurse midwife
- Clinical psychologist
- Clinical social worker
- Registered dietitian
- Nutrition professional
The opt-out law does not define “physician” to include chiropractors; therefore, they may not opt out of Medicare and provide services under private contract.
Physical therapists in independent practice and occupational therapists in independent practice cannot opt out because they are not within the opt-out law’s definition of either a “physician” or “practitioner.”
Posted by
Unknown
at
4:33 PM


Physical Therapists Cannot Opt-Out of Medicare
2012-06-18T16:33:00-04:00
Unknown
chiropractors|First Coast Service Options|Medicare beneficiaries|opt out|Physical therapists in independent practice|physician|
Comments
Labels:
chiropractors,
First Coast Service Options,
Medicare beneficiaries,
opt out,
Physical therapists in independent practice,
physician
Saturday, June 16, 2012
Physical medicine and rehabilitation physicians targeted in probe of therapy services
First Coast Service Options Inc. (FCSO) conducted a widespread probe (WSP) review in response to an aberrant billing pattern for CPT codes and posted this notice June 12th, 2012.
Here are the codes with high error rates:
The most common reason for an error to be assigned was insufficient documentation including failure to meet Medicare’s documentation requirements specific to therapy services.
As a result of the widespread probe findings, FCSO will implement a prepayment medical review edit for therapy services billed by physical medicine and rehabilitation physicians.
The following is a brief summary of Medicare requirements for therapy services:
Documentation in the Patient's Chart
The following documentation must be submitted in response to a request for documentation, unless the requesting contractor specifies otherwise.
Medicare is authorized to pay only for services provided by those trained specifically in physical therapy, occupational therapy or speech-language pathology.
That means that the services of athletic trainers, massage therapists, recreational therapists, kinesiotherapists, low vision specialists or any other profession may not be billed as covered therapy services.
In addition, there is no coverage for services provided “incident to” the service of a therapist. Although physical therapist assistants (PTAs) and occupational therapy assistants (OTAs) work under the supervision of a therapist and their services may be billed by the therapist, their services are covered under the benefit for therapy services and not by the benefit for services “incident to” a physician/NPP. The services furnished by PTAs and OTAs are not incident to the therapist’s services. A physical therapist must supervise PTAs and an occupational therapist must supervise OTAs. The level and frequency of supervision differs by setting (and by state or local law). General supervision is required for PTAs in all settings except private practice (which requires direct supervision) unless state practice requirements are more stringent, in which case state or local requirements must be followed. The service of a PTA and OTA shall not be billed as services “incident to” a physician/NPP’s service, because they do not meet the qualifications of a therapist. Only services provided by a licensed therapist or an individual who has completed an accredited PT or OT curriculum and are qualified for licensure may provide services “incident to” the physician/NPP.
Providers are encouraged to review the complete requirements for billing rehabilitation services found on FCSO’s Therapy and Rehabilitation Services local coverage determination L29399 (Puerto Rico and the U.S. Virgin Islands) as well as the requirements found in the Internet-only manual (IOM), Pub. 100-02 , Medicare Benefit Policy Manual, Chapter 15, Sections 220-230 .
Here are the codes with high error rates:
- 97032 (Application of a modality to one or more areas; electrical stimulation [manual], each 15 minutes);
- 97035 (Application of a modality to one or more areas; ultrasound, each 15 minutes)
- 97124 (Therapeutic procedure, one or more areas, each 15 minutes; massage including effleurage, petrissage and/or tapotement [stroking, compression, percussion]) billed by specialty 25 (physical medicine and rehabilitation).
The most common reason for an error to be assigned was insufficient documentation including failure to meet Medicare’s documentation requirements specific to therapy services.
As a result of the widespread probe findings, FCSO will implement a prepayment medical review edit for therapy services billed by physical medicine and rehabilitation physicians.
The following is a brief summary of Medicare requirements for therapy services:
- Therapy services shall be payable when the medical record and the information on the claim form consistently and accurately report covered therapy services.
- Documentation must be legible, relevant, and sufficient to justify the services billed.
- The patient receiving outpatient therapy services must be under the care of a physician/nonphysician practitioner (NPP). NPP signifies a physician assistant, clinical nurse specialist or nurse practitioner, who may, if state and local law permit it, and when appropriate rules are followed, provide, certify, or supervise therapy services.
- Therapy services must relate directly and specifically to a written treatment plan.
- The plan (also known as a plan of care or plan of treatment) must be established before treatment is started. The plan is established when it is developed (e.g., written or dictated).
- The signature and professional identity (e.g., MD, OTR/L) of the person who established the plan, and the date it was established must be recorded within the plan.
- The Plan of Care shall contain, at minimum, the following information as required by regulation (42 CFR 424.24 and 410.61) See Pub. 100-02, Chapter 15, section 220.3 for further documentation requirements).
- Diagnosis
- Long Term treatment goals
- Type, amount, duration and frequency of therapy services
- The plan of care shall be consistent with the related evaluation, which may be attached and is considered incorporated into the plan.
- The plan should strive to provide treatment in the most efficient and effective manner, balancing the best achievable outcome with the appropriate resources.
- Long Term treatment goals should be developed for the entire episode of care and not only for the services provided under a plan for one interval of care in the current setting.
- When the episode of care is anticipated to be long enough to require more than one certification, the long term goals may be specific to the part of the episode that is being certified.
- Goals should be measurable and pertain to identified functional impairments.
- When episodes in the setting are short, measurable goals may not be achievable; documentation should state the clinical reasons progress cannot be shown.
- The type of treatment may be PT, OT, or SLP, or, where appropriate, the type may be a description of a specific treatment or intervention.
- Where a physician/NPP establishes a plan, the plan must specify the type (PT, OT, SLP) of therapy planned.
The following documentation must be submitted in response to a request for documentation, unless the requesting contractor specifies otherwise.
- Evaluation and plan of care (POC) (may be one or two documents). Include the initial evaluation and any reevaluations relevant to the episode being reviewed; Certification (physician/NPP approval of the plan) and recertification when records are requested after the certification/recertification is due;
- Progress reports (including discharge notes, if applicable) when records are requested after the reports are due;
- Treatment notes for each treatment day (may also serve as progress reports when required information is included in the notes). Daily treatment notes must indicate the individual modalities performed that day. Minutes must be documented for each modality that represents a time-based code and the total time in treatment must be documented.
- A separate justification statement may be included either as a separate document or within the other documents if the provider/supplier wishes to assure the contractor understands the reasoning for services that are more extensive than is typical for the condition treated. A separate statement is not required if the record justifies treatment without further explanation. If the patient is expected to exceed the therapy cap, the record must clearly indicate the medical necessity for the patient to receive covered services above the cap. Note: The excessive use of modifier KX (Requirements specified in the medical policy have been met) may indicate abusive billing.
Medicare is authorized to pay only for services provided by those trained specifically in physical therapy, occupational therapy or speech-language pathology.
That means that the services of athletic trainers, massage therapists, recreational therapists, kinesiotherapists, low vision specialists or any other profession may not be billed as covered therapy services.
In addition, there is no coverage for services provided “incident to” the service of a therapist. Although physical therapist assistants (PTAs) and occupational therapy assistants (OTAs) work under the supervision of a therapist and their services may be billed by the therapist, their services are covered under the benefit for therapy services and not by the benefit for services “incident to” a physician/NPP. The services furnished by PTAs and OTAs are not incident to the therapist’s services. A physical therapist must supervise PTAs and an occupational therapist must supervise OTAs. The level and frequency of supervision differs by setting (and by state or local law). General supervision is required for PTAs in all settings except private practice (which requires direct supervision) unless state practice requirements are more stringent, in which case state or local requirements must be followed. The service of a PTA and OTA shall not be billed as services “incident to” a physician/NPP’s service, because they do not meet the qualifications of a therapist. Only services provided by a licensed therapist or an individual who has completed an accredited PT or OT curriculum and are qualified for licensure may provide services “incident to” the physician/NPP.
Providers are encouraged to review the complete requirements for billing rehabilitation services found on FCSO’s Therapy and Rehabilitation Services local coverage determination L29399 (Puerto Rico and the U.S. Virgin Islands) as well as the requirements found in the Internet-only manual (IOM), Pub. 100-02 , Medicare Benefit Policy Manual, Chapter 15, Sections 220-230 .
Posted by
Unknown
at
6:22 AM


Physical medicine and rehabilitation physicians targeted in probe of therapy services
2012-06-16T06:22:00-04:00
Unknown
documentation|Medicare|physical medicine and rehabilitation physicians|physical therapy|Plan of Care|therapy services|
Comments
Labels:
documentation,
Medicare,
physical medicine and rehabilitation physicians,
physical therapy,
Plan of Care,
therapy services
Subscribe to:
Posts (Atom)
Free Tutorial
Get free stuff at BulletproofPT.com
Tim Richardson, PT owns a private practice at Medical Arts Rehabilitation, Inc in Palmetto, Florida. The clinic website is at MedicalArtsRehab.com.
Bulletproof Expert Systems: Clinical Decision Support for Physical Therapists in the Outpatient Setting is a manager's workbook with stories, checklists, charts, graphs, tables, and templates describing how you can use paper-based or computerized tools to improve your clinic's Medicare compliance, process adherence and patient outcomes.
Tim has implemented a computerized Clinical Decision Support (CDS) system in his clinic since 2006 that serves as a Reminder, Alerting, Prompting and Predicting CDS using evidence-based tests and measures.
Tim can be reached at
TimRichPT@BulletproofPT.com .
"Make Decisions like Doctors"
Copyright 2007-2010 by Tim Richardson, PT.
No reproduction without authorization.
Bulletproof Expert Systems: Clinical Decision Support for Physical Therapists in the Outpatient Setting is a manager's workbook with stories, checklists, charts, graphs, tables, and templates describing how you can use paper-based or computerized tools to improve your clinic's Medicare compliance, process adherence and patient outcomes.
Tim has implemented a computerized Clinical Decision Support (CDS) system in his clinic since 2006 that serves as a Reminder, Alerting, Prompting and Predicting CDS using evidence-based tests and measures.
Tim can be reached at
TimRichPT@BulletproofPT.com .
"Make Decisions like Doctors"
Copyright 2007-2010 by Tim Richardson, PT.
No reproduction without authorization.